Autism and acetaminophen (paracetamol) use in pregnancy - the evidence
The press conference in the USA yesterday raised a concerning question - does the use of acetaminophen (paracetemol) cause autism?
I feel it is important to look at the larger picture here - so I will share what we know, what we are not so clear about and how best to move forward without portioning blame on yourself or others.
Let’s start with the thing we know for sure – there is not one, single, ‘root cause’ of autism. Research points to an underlying genetic susceptibility, with multiple factors influencing each individual, including:
medications
environmental toxins
maternal infections
immunological factors
mitochondrial dysfunction
methylation dysfunction
nutrient deficiencies
gut microbiome
inflammation and allergies.
Some studies support the claim that paracetamol use in pregnancy may be associated with a likelihood of autism or ADHD, while other studies find no link.
In clinical practice I see patients whose mums used paracetemol during pregnancy, and their children did not develop autism. And I have patients who were never exposed to paracetemol or vaccines, and still developed autism.
As stated above - there is no single cause for autism, there are many and it is complex and individual. There is still so much research being undertaken and needs to be undertaken. What is important here is that no one should feel guilty or portion blame for decisions they made, with the information they had available at the time.
There are studies supporting both opinions:
Some studies show increased risk: A 2025 systematic review of 46 studies found that higher-quality research more often showed a link between prenatal acetaminophen exposure and increased likelihood of autism or ADHD.(1)
Some studies show no risk: A Swedish cohort of nearly 2.5 million children found no increased likelihood when comparing siblings (which controls for shared genetics and environment).(2)
Cord blood study: In the Boston Birth Cohort, higher cord blood acetaminophen metabolites were linked to increased likelihood of autism and ADHD.(3)
What and how - the simple biochemistry explanation
Acetaminophen depletes glutathione — the master antioxidant in the body and champion detoxifier. When glutathione is low, oxidative stress rises, which can affect brain development.(4)
What we still don’t know
Cause and effect - confounding factors like fever, infection, dose, and timing during pregnancy all need consideration
We don’t yet know which trimesters or doses carry the most risk, or which children are most vulnerable because of their genetic susceptibilities.
Education = empowerment - what you can do now:
Use acetaminophen only when really necessary - keep yourself and your child within safe limits of fevers, but understand the role of a fever in the body - it is not something to be feared.
Learn about alternatives that reduce the need for acetaminophen. For fevers there are many evidence-based options including homeopathy, essential oils, and acupressure points. .
If you do use acetaminophen, support glutathione levels:
Sulfur-rich foods (broccoli, cauliflower, Brussels sprouts, kale, onions, garlic)
Vitamin C-rich fruits
Epsom salt baths
Glutathione supplements when extra detox support is needed. Consult a healthcare practitioner for guidance on dosages.
Key takeaways
Autism and ADHD are not caused by one thing - both conditions are complex and multifactorial.
Acetaminophen may play a role in some genetic susceptible children, but the bigger picture includes the hereditary component, microbiome, environmental toxins, methylation, mitochondrial function, and nutrients
Don’t blame yourself for decisions you made with what you knew at the time. Focus on what you can do: support detox and glutathione, ensure you’re nurturing the microbiome and limit exposure to environmental triggers (see blog on Reducing the chemical load).
Every child with and without autism is unique, with their own strengths and challenges. These studies are not about finding one thing that causes autism and therefore we can simply remove and it’s cured. We are seeking ways to support children who may need extra help with speech and language, learning and motor dysfunction, and/or daily functioning.
References:
Baccarelli A, et al. Environ Health. 2025;24(1):22.
Ahlqvist VH, Sjöqvist H, Dalman C, et al. JAMA. 2024;332(5):452-461.
Ji Y, Azuine RE, Zhang Y, et al. JAMA Psychiatry. 2020;77(2):180-189.
Chen Y, et al. Int J Mol Sci. 2025;26(17):8585.
How to introduce solids and prevent food allergies in infants
For years the advice was - WAIT….Wait until 6 months, wait with allergenic foods, wait with days in between food introduction.
Food allergy prevention - when and how to introduce foods to children is an important conversation we have with families. I get many parents in clinic asking when they should introduce foods, in what order, do they avoid allergenic foods, and the advice out there isn’t always clear.
In recent years the evidence has shifted, and it started with a study in 2015.
The LEAP study (Learning Early About Peanut allergy) demonstrated that introducing peanut products to high-risk infants (those with severe eczema and/or egg allergy) at a young age, between 4 and 11 months, significantly reduced the risk of developing peanut allergy by age five. This landmark randomised controlled trial, shifted the understanding of food allergy prevention from avoidance to active, early introduction.
The publication of the LEAP findings led to rapid changes in infant feeding and allergy prevention guidelines around the world to recommend early peanut introduction. Some guidelines focused only on early peanut introduction, while others also recommended early introduction of egg, which was shown in meta-analyses of randomised controlled trials to reduce the risk of egg allergy. Although there is currently insufficient evidence from randomised controlled trials to guide recommendations around introduction of other allergenic foods such as tree nuts, several guidelines recommend introduction of a wide variety of allergenic foods in the first year of life based on the hypothesis of a similar mechanism of protection irrespective of the allergen in question.
In response to the LEAP findings, the Centre for Food and Allergy Research, the Australasian Society of Clinical Immunology and Allergy, and the Australian National Allergy Strategy hosted an Australian Infant Feeding Summit in 2015 to appraise the new evidence and developed revised recommendations for infant feeding.
Three recommendations:
introduce solid foods around 6 months of age, but not before 4 months
introduce allergenic foods including peanut butter and cooked egg in the first year of life
hydrolyzed infant formula is not recommended for the prevention of allergic disease.
The consensus aimed to provide consistency between different Australian guidelines to ensure clear consumer advice while balancing the need for food allergy prevention with other nutritional priorities, including the known benefits of breastfeeding. These recommendations were incorporated into the Australasian Society of Clinical Immunology and Allergy’s infant feeding guidelines in 2016.
Take aways
The landmark LEAP study and multiple follow-ups now show that early introduction of allergenic foods—especially between 4–6 months—significantly reduces the risk of severe food allergies.
The wait model is not only unsupported, it may actually increase allergy risk.
Other nutritional, environmental and genetic factors need to be considered on a case by case basis.
References:
preventallergies.org.au/the-learning-early-about-peanut-allergy-leap-study
Koplin JJ, Soriano VX, Peters RL. Real-World LEAP Implementation. Curr Allergy Asthma Rep. 2021 Jun;22(6):61-66.
L-theanine - use in children for sleep, focus and anxiety
L-theanine, an amino acid found in green tea is known for promoting relaxation without sedation. We are often looking for safe, effective and evidence-based options to support our kids with focus, sleep quality, and emotional health, and evidence shows this nutrient may be worth adding to the mix.
With a molecular structure similar to glutamate, a neurotransmitter involved in brain function, theanine is known for its ability to cross the blood-brain barrier and exert various neurophysiological effects. It is believed to promote relaxation without causing drowsiness, which has led to its widespread use as a supplement aimed at reducing stress and anxiety. Research suggests that theanine increases the production of alpha waves in the brain, associated with a state of relaxed alertness, and may enhance cognitive function and attention, particularly when combined with caffeine.
Here’s what the evidence says:
Sleep support in ADHD: 400 mg/day improved sleep efficiency in children aged 8–12 with ADHD, with no significant adverse effects.
Attention & calm: L-theanine (alone or with caffeine) improved sustained attention and inhibitory control in children with ADHD.
Anxiety & tics: A pilot study combining L-theanine with vitamin B6 showed reduced tic severity and anxiety in children with Tourette’s.
Functions of theanine
Theanine is probably known best for its stress relieving properties. In addition to this, it is also:
antioxidant
anti-inflammatory
neuroprotective
anti-cancer
immune boosting
metabolism regulating properties.
It’s also been shown to protect the heart, liver, kidneys from oxidative stress, and support gut health by decreasing intestinal pressure, reducing inflammation, and providing antioxidant activity. Pretty impressive list huh :-)
Doses
There isn’t an established RDA for theanine since it isn’t required for our survival. Before adding doses in supplement form, be sure to consult with a qualified healthcare professional to ensure no contraindications with other things you may be taking or any health conditions you may have.
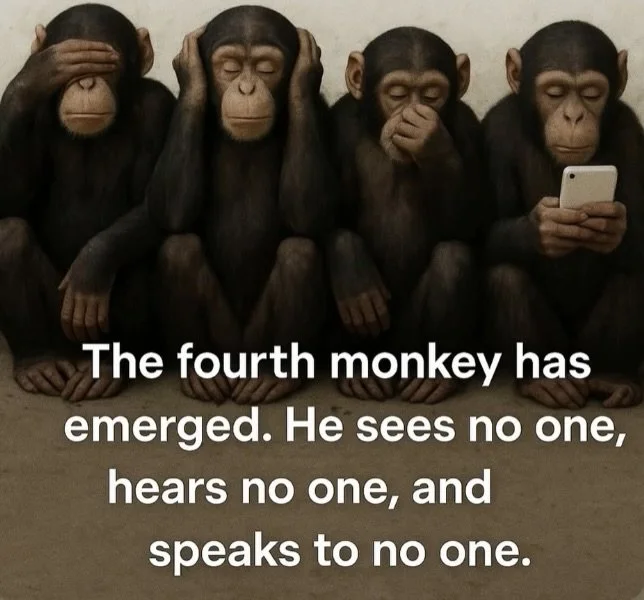
The impact of your technology use on your child’s health and development
Yep…it’s not just their direct screen time….it’s your use of technology whilst you’re in their presence that’s having an impact too….it’s coming at them from all fronts! Children are sponges in their younger years, both mirroring your behaviours and absorbing what and how you respond in situations. 70%+ of language is unspoken…so your behaviours and ‘presence’ really counts.
This systematic review and meta-analysis included data from 21 studies across nearly 15,000 children under age five years. Researchers examined associations between parental screen use during caregiving moments and a range of child outcomes.
Key takeaways
➣ Cognitive development: Slightly lower scores in attention, problem-solving, and related domains (r ≈ –0.14).
➣ Emotional & behavioural health: Higher internalising (anxiety/depression) and externalising behaviors (r ≈ +0.13 to +0.15).
➣ Social skills: Modestly lower prosocial behaviours and weaker attachment signals (r ≈ –0.08 to –0.10).
➣ Screen time patterns: Children tended to have more screen time themselves when parents modelled higher tech use (r ≈ +0.23).
All associations were statistically significant but small—pointing to a pattern rather than a cause.
Clinical implications
For paediatric providers, this research underscores the value of asking about parental tech habits during early childhood visits—not just kids’ screen time.
Small reminders about mindful device use and creating tech-free family times can be an approachable way to support cognitive, emotional, and relational health in young children.
This isn’t about adding stigma or guilt—rather, helping families notice habits that may otherwise go unaddressed.
Screen use and children's social and emotional wellbeing
Electronic screens are everywhere and are easily accessible to children. But what impact are they having on our children’s health and wellbeing?
Electronic screens are everywhere and are easily accessible to children. Almost every parent I see in clinic reports concerns that screens are ‘an issue’ in their household, and are concerned about the socio-emotional problems they may be causing their children.
A recently published study (see ref below) looked at 292,739 children across 117 studies and the overall conclusions were that screen use led to socio-emotional problems and socio-emotional problems led to greater screen use, with gaming behaviour being the more significant factor.
Social and emotional wellbeing is pivotal to children’s health, reflecting how they feel, behave, and cope with challenges. Children are said to have socio-emotional disorders when how they feel and what they do differ from the expectations of their developmental stage - such as aggression, withdrawal, or anxiety.
Children and adolescents spend an increasing amount of time on electronic screens for entertainment, homework, and socialisation with friends . A meta-analysis on the global prevalence of screen use among children found that three in four children younger than two years were being allowed screens, despite guidelines recommending they wait until two years.
Screen use grows as children get older. For example, among those aged 2–5 years, one in three children exceed screen time limits of 1 hr per day. A USA report showed that about half of American children aged 2–4 years had their own tablet or smartphone, and more than two thirds of 5-8 year olds. These 5-8 year olds spent an average of 3 hr per day on screens. Among older children (8–12 years), these numbers were even more concerning: 41% spend more than 4hrs per day using screens and 15% more than 8hrs per day.
Computers, televisions, smartphones, and tablets can all be used for different purposes (e.g. gaming, social media, entertainment, learning). Researchers have long identified that different content (e.g. Sesame Street vs. advertising vs. social media) has different effects, and they have increasingly explored the outcomes from different devices.
Children with TVs in their bedrooms engage less in non-electronic family activities (e.g. playing board games) compared to those without a TV in their own room.
Screen use therefore appears to displace opportunities to be physically active, to have regular and good-quality sleep, and to have positive social interactions with family and peers.
There is also the biopsychosocial model, which explains how socio-emotional problems can develop from deficits in physical needs such as sleep and physical activity. as we know, sleep is critical for emotional regulation and cognitive functioning, and when screen time disrupts sleep patterns, it can lead to increased anxiety, mood disturbances, and difficulties in emotional regulation. Similarly, physical activity is essential for reducing stress and promoting mental health. Therefore, one theory connecting screens and socio-emotional problems is how they displace protective behaviours - mainly sleep and physical activity.
The study showed there is moderate difference at different ages by gender. Across the whole sample, girls were at greater risk of developing socio-emotional problems following their interactions with screens. However, when looking at older children only, boys seemed at greater risk than girls. Specifically, compared to older girls, older boys were more likely to present socio-emotional problems over time and more likely to turn to screens when facing socio-emotional problems.
Conclusions
The study findings suggest that while all parents should be vigilant about their child’s gaming interactions—i.e. prioritising educational games and ensuring that recreational games are age-appropriate—the focus should intensify as children enter later developmental stages. Parents and policymakers need to consider a proactive approach to supporting children with socio-emotional difficulties. They may limit game use more tightly than educational screen time to prevent gaming from becoming a maladaptive coping mechanism.
Importantly, parenting style matters , even in the way parents put boundaries around screens: research indicates that an autonomy-supportive style of communicating gaming rules is generally more effective than a controlling approach . Managing screen use is just one of many strategies parents can use to prevent socio-emotional problems. Including interventions that foster positive peer relationships and family dynamics, enhance social skills, or provide emotional support are all valuable too. It is recommended that parents remain actively involved in their child’s gaming interactions for as long as possible. This continued involvement may help strengthen parent–child relationships, mitigating the chances of children becoming compulsive gamers. By doing that, parents and caregivers can help create a more supportive environment that addresses the root causes of problematic gaming and socio-emotional problems.
Screen time guidelines should focus not just on limiting use, but also on encouraging positive content, social interaction, and reducing high-risk behaviours like excessive gaming.
Public impact statement from the study:
Our review found that screen use can contribute to socio-emotional problems, and children with these problems are more likely to use screens as a coping mechanism. The effects appeared stronger for gaming. These links highlight the need for close attention from parents, researchers, and policymakers. Our findings support screen time guidelines that not only limit exposure time but also emphasise content quality and a positive social context. Parents should consider monitoring not just how long children are on screens, but also what they are doing and who they are interacting with. Some types of screen use, like coviewing with parents, seem to have few harms, if any. Parents may be able to avoid a cycle of screen use by supporting their socio-emotional development in other ways.
Ref:
https://psycnet.apa.org/fulltext/2026-24348-001.html
It’s life Captain, but not as we know it…
Every time I see new research on the gut-brain interaction and the role of bacteria, the image that always pops in to my head is a bridge on a cool spaceship being captained and controlled by cute, colourful ‘bugs’ :-)
As we are often reminded with this research, our gut is a bustling and thriving alien colony – trillions of bacteria from thousands of species, and many were here long before humans. They outnumber our human cells many, many times over.
Collectively, these microbial armies are known as the "microbiota" – and they play a well-established role in maintaining our physical health, from digestion and metabolism to immunity. They also produce vital compounds the human body is incapable of manufacturing on its own. And we now know, they also travel at a vast speed to our brains – like a hotline to our minds.
Over the last few decades, researchers have started to uncover curious, compelling – and sometimes controversial – evidence to suggest that the gut microbiota doesn't just help to keep our brains in prime working order by helping to free up nutrients for it from our food, but may also help to shape our very thoughts and behaviour. Their findings may even potentially bolster how we understand and lead to new treatments for a range of mental health conditions, from depression and anxiety to schizophrenia.
What’s kinda cool, is this modern-day research stems from a point of origin story from 1822! We won’t share the graphic details, but suffice to say, the doctor at the time studied a gut noting the gastric contents were affected by the owner’s emotions. Through this the Dr proposed the idea of a gut-brain axis. And now we know that the microorganisms within our gut make this process even more complex and remarkable.
Dr Beaumont with patient Alex St. Martin in 1822
Recent research out of the USA, shows more insights in to how specific gut microbes can modulate the immune system in ways that impact the brain and also produce molecules that signal directly to neurons to regulate their activity. Gut microbes can regulate the early development of neurons in ways that lead to long-lasting impacts on brain circuitry and behaviours.
On a more regular, short-term basis, gut microbes regulate the production of many biochemicals including serotonin – showing that these microbes are communicating with our brains through many pathways.
The good news is that you can change your microbiota, you are in control of it. Pro- and prebiotic supplements, simple dietary changes, such as eating more fibre and fermented foods, along with lifestyle activities such as meditation and exercise – can help alter our microbiota in ways that benefit our minds.
With many studies underway isolating specific pre- and probiotics that impact mood and behaviour, the aim is to use them as psychobiotics to nurture populations of "good" bacteria – and treat a variety of mental health conditions, as an adjunct to current medications or…here’s hoping….an alternative.
https://www.bbc.com/future/article/20230120-how-gut-bacteria-are-controlling-your-brain
Reducing the chemical load
As we know, the cause of autism spectrum disorders (ASD) is multifactorial, but a recent study(1) has presented a hypothesis suggesting that exposure to toxins may affect individuals with genetic susceptibility.
The study examined two compounds: Bisphenol-A (BPA) and Diethylhexyl Phthalate (DEHP), both commonly used in the production of plastics, the manufacture of PVC, and in the resins that line many food and drinks containers. Whilst the primary route of exposure is through diet, inhalation and personal care products also play a part.
Some studies(2) have shown evidence of a link between plasticiser exposure and neurodevelopmental disorders, with several mechanisms have been proposed, such as plasticisers acting as endocrine disruptors(3,4). This recent study has hypothesised that the connection is due to a genetic inability to detoxify plasticisers like BPA through the metabolic and excretion pathways that make the substances water soluble so they can be eliminated through urination.
The study has theorised that detoxification of these compounds is impaired in children with ASD and ADHD. They assessed this by examining the detox pathways in three groups of children: 66 with ASD, 46 with ADHD, 37 healthy controlsresults showing that detox efficiency for BPA was reduced by 11% in children with ASD and 17% in children with ADHD compared to controls. DEHP followed similar trends, though the differences were not statistically significant. The study concluded that both ASD and ADHD share a reduced capacity for detoxifying BPA and DEHP, with the reduction in BPA detoxification being statistically significant.
Changes you can make to reduce your family’s exposure to toxins
1. Simple living
a. Eat unprocessed food
b. Avoid canned foods and artificial food additives
c. Walk or cycle to work
d. Buy second hand
e. Lend and borrow
f. Limit use of medications where possible
g. Fill your house with fresh air and furniture made from natural materials
h. Come back to nature at every opportunity
2. Buy organic
a. Significantly reduces chemical exposure – GMOs, pesticides and fertilisers
b. Follow the EWG’s dirty 12 and clean 15 www.ewg.org
c. Avoid chemical exposure in seafood, eat low-mercury fish – know where your fish has come from
3. Reduce your use of personal care products, make up and perfume
a. Simplify your beauty regime
b. Avoid face and body scrubs using microbeads, foaming agents like sodium-laurel-sulfate and preservatives such as parabens
c. Go natural with all body-care products
d. Avoid nail polishes and removers, aerosols, conventional hair dyes whilst pregnant or breast feeding
e. Be careful what you put on baby’s skin. Choose brands such as www.moogoo.com.au
4. Minimise the number of household cleaners you use
a. Find a natural alternative for your cleaning products e.g. www.zeroco.com
b. Avoid use of insecticides/pesticides in home or garden, kill bugs naturally or just allow yourself to become one with nature
5. Ditch perfumes and artificial fragrances
a. Air fresheners, fabric softeners, scented candles and soaps, cheap incense all contain synthetic fragrances (phthalates) which are hormone disruptors
b. Opt for fresh flowers, essential oils (make sure they are pure)
c. Limit perfume use and if you must use, spray on clothes not skin
6. Move away from plastic
a. Don’t store food or drinks in plastic – containers, bags, water bottles, coffee cup lids
b. Store in glass or steel
c. Don’t microwave ANYTHING in plastic
d. Use paper towel rather than clingwrap or better still, beeswax wraps
e. Ensure you are looking for BPA-free bottles for babies, children and yourself
7. Avoid toxic cookware
a. Non-stick cookware is toxic! Avoid Teflon
b. Opt for cast iron, steel, ceramic and oven-safe glass
8. Drink filtered water
a. Filters can reduce levels of many pollutants
b. Reverse osmosis is highly effective, but high-quality charcoal filters are also great in free-standing filters if you can’t have a RO filter fitted
Little decisions can have a big impact on you and your family’s cumulative chemical exposure. Don’t feel overwhelmed by this very large, often daunting topic. Just keep moving forward, one small change at a time.
Reference:
1. Stein TP, et al. PLoS ONE. 2023;18(9): e0289841.
2. Minatoya M, Kishi R. Int J Environ Res & Pub Health. 2021;18(7):30.
3. Flaws J DP, et al. A guide for public interest and policy-makers on endocrine disrupting chemicals and plastics. Endocrine Society. 2020. Available at: https://www.endocrine.org/-/media/endocrine/files/topics/edc_guide_2020_v1_6bhqen.pdf. Accessed on: 17/10/24
4. MacKay H, Abizaid A. Hormones & Behavior. 2018;101:59–67. pmid:29104009
Gastrointestinal health in autism spectrum disorder
Children with autism spectrum disorder (ASD) are at higher risk of medical issues, and more prone to gastrointestinal (GI) disorders, which can worsen the symptoms of ASD symptoms – significantly affecting their health, learning and development, and impacting their behaviour.
GI issues may include:
food intolerances
constipation
inflammatory bowel disease (IBS/IBD).
The causes of GI disorders can include gut dysbiosis, immune dysfunction, food sensitivities, digestive enzyme deficiencies, and sensory processing differences. Selective eating habits can also lead to unbalanced diets and bring on, or exacerbate GI problems.
Diagnosing GI issues in ASD can be difficult as there are often communication issues and there are a lack of clinical guidelines in this area.
As a parent, you are most likely to notice changes or behaviours in your child which are possibly linked with a GI issue. These include, but are not limited to:
showing unusual postures – hanging over the side of furniture, walking with a bent posture
sleep problems and nightmares
food intolerances – new food reactions or sensitivities. These will often show up as tummy upsets, skin rashes or feelings of nausea
aggressive behaviours
attention issues.
Treating GI disorders has been shown to improve ASD symptoms.
When pursuing any testing with your healthcare practitioners, ensure to look for coeliac/gluten sensitivity – whilst coeliac is not more common in ASD, there is an overlap. Work with your healthcare practitioner if considering removing any food groups from your child’s world, to ensure no further nutrient depletion occurs.
Understanding the nuances of diet and GI health in your child is key to improving outcomes. Dietary management of GI symptoms can improve digestion, nutrient absorption, and appetite by reducing physical discomfort and pain, as well as relieving GI symptoms which will then improve sleep, boost energy levels, and contribute to overall wellbeing, leading to a better quality of life and improved family dynamics.
Reference:
Al-Beltagi M, et al. World J Clin Pediatr. 2023;12(4):171-196.
Sing (or eat) a rainbow
Red and yellow and pink and green…..yes, it’s the rainbow song! And…a great way to think about getting some food diversity in to your selective eaters.
Rainbow smoothies as a breakfast choice or snack are a fabulous way to get your kids involved in food prep and choice, as well as hiding a myriad of goodness without them ever suspecting - veggies, seeds, nuts, fibres…
Here are a few recipes to get you started:
· Red: milk of choice, coconut water or water, 1 cup berries fresh or frozen (strawberries, raspberries), 1 tablespoon chia seeds, 1 tablespoon flaxseeds, 1/4 avocado, ½ zucchini (raw or steamed)
· Purple: milk of choice, coconut water or water, 1 frozen banana, 1/2 raw beetroot peeled, 1/2 cup frozen berries, 1/2 avocado, 1 tablespoon chia seeds, 1 tablespoon hemp seeds
· Green: milk of choice or coconut water, 1 x kiwi, handful spinach, ½ zucchini (raw or steamed), 1 tablespoon chia seeds, 1 tablespoon hemp seeds, 1/4 avocado
o Another option here is choc/mint – add 1 teaspoon raw cocoa power and a handful of mint to the above
· Yellow: milk of choice, coconut water or water, 1 x banana, ¼ cup oats, ½ carrot, ½ cup frozen mango and/or 1 x passionfruit, 1 tablespoon chia seeds, 1 tablespoon hemp seeds
You can add anything to smoothies, but aim for max 2 x fruit and always put some vegetables in there along with the seeds. Add honey to taste if they need to be a little sweeter.
You can also replace the water content with yoghurt if a thicker, creamer texture is preferred.
Whizz it all up in a food processor, and adjust the quantities to fit your chosen blender.
Enjoy!
Household mould – is it a health hazard?
Mould - it’s winter and therefore ‘mould season’. Here’s some insights and tips to help keep your house as mould free as possible.
As winter hits all parts of Australia, here in the west, we get the most rain in these few months….and the most humidity. And by definition….the highest risk of mould.
Whether it's the slimy black spots on your shower curtain, the fuzzy white patches on your walls, or the slick orange film that forms on your kitchen sink, household mould is more than just ugly, it can make you sick.
Mould is insipid fungus, toxic and dangerous. It needs treating at the source, by the right cleaning solutions, and, if serious, by a building biologist (mould expert).
The list of infections, symptoms and conditions can include:
- sinus issues
- skin infections
- yeast infections
- respiratory infections and exacerbation of asthma
- headaches
- aching joints
- asthma
- fatigue
- loss of libido
- depression and anxiety
- slow wound healing
Connecting the dots with symptoms and mould can be a long, drawn-out process as the symptoms can be so many other things, and, the mould is not always seen in your house for you to even realise it is there.
Mould thrives in damp and humid conditions, in places that are not well ventilated. These conditions are often exacerbated along Australia's eastern seaboard with damp, humid summers.
Some tips for controlling mould
It's impossible to get rid of all mould and mould spores in your home, but because mould spores can't grow without moisture, reducing moisture in your home is the best way to prevent or eliminate mould growth.
If there is already mould growing in your home, it's important to clean up the mould and fix the problem causing dampness. If you clean up the mould but don't fix the problem, the mould will return.
If the mould is very bad, you may need to consider a building biologist to come in and assess and fix the problem.
Tips for reducing moisture in your home:
Use dehumidifiers and air conditioners to reduce moisture in the air
Keep indoor humidity below 60% if possible
Add insulation to cold surfaces, such as exterior walls, floors, and windows to reduce condensation
Dry wet areas within 24 to 48 hours to prevent mould growth
Open windows and doors to increase circulation. Increase air circulation by using fans and moving furniture from wall corners
Use exhaust fans to move moisture outside whenever you are cooking, using tumble dryers, or cleaning
Check for leaks around the kitchen and bathroom sinks, refrigerators and other sources of water
Iron – an important mineral for our kids
Iron – an important mineral for our kids
Iron is a very important mineral for our children during the critical stages of childhood development. From the day they are born through to adolescence, children require enough iron to fuel their growing bodies and brains. Iron is important for:
- Energy production: iron is vital to the function of haemoglobin, a protein needed to transport oxygen in the blood to muscles and the brain so is crucial for mental and physical performance.
- Cognitive development and function: iron is needed for healthy brain development and function, and has a key role in the production of the neurotransmitters. serotonin, dopamine and norepinephrine, needed to optimise learning, memory, and focus.1
- Cognitive impairment: research shows that iron deficiency in children can lead to cognitive impairments, including poor learning difficulties, depression, attention and concentration.1
- Immune function: iron plays an important role in helping to fight off infections and illnesses through recruitment of our ‘fighter cells’ – regulating innate and adaptive immunity.2 Healthy iron levels are essential for maintaining a strong immune response and warding off infections in our children.
- Delayed growth: iron is important in children’s growth and development, leading to delays in physical milestones.3
Types of iron
Iron comes in two different forms: heme and non-heme iron.
- Heme iron is readily absorbed by the body and comes from animal sources.
- Non-heme iron is not absorbed as easily because it interacts with other food components like phytates and oxalates, which reduce how well the body absorbs it. Non-heme iron comes from plant sources.
Including a variety of both heme and non-heme iron sources helps create a well-balanced diet, and ensures they meet their iron requirements for optimal growth and development.
Heme iron sources: animal foods are the best way to get heme iron in to your children.
- Lean meats: beef, lamb and kangaroo are rich sources of heme iron and provide essential protein for growth and development
- Fish and seafood: salmon, tuna, mussels, anchovies, and other seafood, while not as rich in iron as red meat, are still a good source and in addition, provide omega-3 fatty acids for brain health
- Eggs and dairy products: eggs and cheese have less iron content than meat, but they are still valuable sources of heme iron, calcium, and other essential nutrients.
Non-heme iron sources: plant-based foods contain non-heme iron. It is not as readily absorbed as heme iron, but it can still add plenty of iron to your child's intake. Plant-based, iron-rich foods for vegetarian kids are essential as they are the only source of dietary iron.
- Legumes: lentils, white beans, chickpeas, and peas
- Whole grains: quinoa, oats, brown rice, and fortified cereals
- Nuts and seeds: almonds, pumpkin seeds, sunflower seeds, and nut butters are rich in iron
- Dark leafy greens: spinach, kale, swiss chard, and broccoli have good amounts of iron
- Fortified foods: many processed foods, such as cereals, bread, and plant-based milks, are fortified with iron.
Iron absorption
As well as including adequate amounts of iron-rich foods in your child’s diet, there are also some tricks you can use to improve the absorption and make sure they’re getting the most out of their meal. Here are some tips on how to maximise iron absorption:
- Eating iron-rich foods with vitamin C - incorporating vitamin C-rich foods alongside non-heme iron sources may improve absorption. Vitamin C enhances uptake by converting non-heme iron into a more absorbable form. Here are some food suggestions:
o Citrus fruit: oranges and lemons are great sources of vitamin C. Try adding a squeeze of lemon juice to salad or green beans.
o Berries: strawberries, blueberries, raspberries, and blackberries are full of vitamin C and antioxidants. Include them alongside a handful of nuts for a balanced snack.
o Tomatoes: all forms of tomatoes are good sources of vitamin C. Baby tomatoes are a great snack in lunchboxes, or dice up fresh toms and make a sauce for your bolognese.
o Capsicum: all colours of capsicums are rich in vitamin C. Include some sticks of capsicum with a dip for afternoon tea or in a stir-fry.
Foods and drinks that may restrict iron absorption
On the flip side, there are certain foods and drinks that may restrict iron absorption and need to be consumed in moderation when eating iron-rich foods. These include:
- High-calcium foods like milk and yoghurt
- Foods high in tannins like tea and coffee – not usually an issue with children.
Daily iron requirements in children
Age, gender, dietary habits, and underlying health conditions all influence iron absorption and the way it is used in the body. To ensure your child meets their daily iron needs to support their growth and development, below is an estimate of recommended dietary intake:4
- Babies (0-6 months): 0.2mg/day
- Infants (7-12 months): 11mg/day
- Toddlers (1-3 years): 9mg/day
- Children (4-8 years): 10mg/day
- Children (9-13 years): 8mg/day
- Teenage boys (14-18): 11mg/day
- Teenage girls (14-18): 15mg/day
Infants need more than toddlers due to their rapid growth, and teenage girls need more than boys due to the onset of periods.
Iron in foods
There are lots of yummy choices that are great iron-rich foods for kids, and suitable for all ages. Below is a selection to give you some ideas.
1 cup cooked lentil = 6.6mg
1 cup white beans = 6.6mg
1 cup cooked spinach = 6.4mg
100g lamb = 3.7mg
1 cup oats = 3.5mg
100g steak = 3.3mg
can of sardines = 3.2mg
1 cup kidney beans = 3.1mg
1/4 cup pumpkin seeds = 3mg
2 x Weetbix biscuits = 3mg
100g tofu = 2.9mg
1 cup quinoa = 2.8mg
1 cup wholemeal pasta = 2.3mg
100g chickpeas = 1.8mg
1 x medium based potato = 1.8mg
20 x cashews = 1.5mg
100g salmon = 1.3mg
can of tuna = 1.1mg
1 x large egg (700-800g) = 1.1mg
30 x almonds = 1.1mg
5 x dried apricots = 1g
1 cup broccoli = 1g
100g chicken = 0.9g
1 slice wholegrain bread = 0.4g
Supplementing
Food-first is the best way of incorporating iron-rich foods in your child's diet. But for selective eaters or other children at risk of iron deficiency, iron supplements are sometimes required.
Before considering an iron supplement for kids, please consult with your GP to assess current iron levels. They will then advise on appropriate dosage and duration if a supplement is needed. Please note: excessive iron intake can be harmful, so careful monitoring is needed.
If supplementation is recommended, choosing a high-quality, child-friendly product is key to ensuring safety and effectiveness – there are liquid and capsule options available to assist in compliance.
References:
1. Berthou C, et al. E J Haem. 2022;3(1):263-275.
2. Ni S, et al. Front Immunol. 2022;13:816282.
3. Cerami C. Ann Nutr Metab. 2017;71(Suppl3):8-14.
4. Nutrient Reference Values for Australia and New Zealand. Available at: https://www.eatforhealth.gov.au/nutrient-reference-values/nutrients/iron. Accessed on: 1/5/24.
Food and mood – part 1
What we eat affects how our gut and brains work.
What we eat affects how our gut and brains work.
How? Well, our guts (enteric nervous system) and our brains (central nervous system) talk to each other via the gut brain axis….like a super highway. And, like a super highway, we want to keep the traffic flowing and happy in both directions.
All sorts of body processes like inflammation, oxidative stress (when there are too many unstable molecules called free radicals in the body and not enough antioxidants to get rid of them. This can lead to cell and tissue damage) and imbalance of good-bad gut bugs can influence how the traffic flows, and our diet is the main influencer.
There is a lot of evidence coming through showing that nutrition and lifestyle changes can be very supportive to individuals with neurodivergence (1-3). In ADHD for example, many individuals have disrupted digestion, and restoring balance in the gut is a key focus from a natural medicine perspective.
The following are also important nutritional and lifestyle factors:
Balancing blood sugar
Identifying food allergies, such as gluten and dairy
Addressing nutrient deficiencies
Ensuring an optimal intake of essential fats, mainly omega 3 fatty acids.
Food is more than just a way of sustaining us. It can be a source of comfort, a treat or bribe and a way of socialising. As a family, the focus therefore needs to be on the general healthiness of the foods. As we see everywhere, diets containing high levels of refined sugar and saturated fat can increase the risk of impulsiveness and hyperactivity, and science is catching up in this space too.
High intakes of refined carbohydrates, sugars and salt, total and saturated fats, and lower intake of omega-3 fatty acids, fibre and folate (vit B9), showed a higher prevalence of ADHD core symptoms.(3)
For example, studies have shown colourings and preservatives have negative effects on the behaviour of children with or without ADHD(4) and the Food Standards Agency(5) list the six food colours most closely linked to hyperactivity in children are:
E102 (tartrazine)
E104 (quinoline yellow)
E110 (sunset yellow FCF)
E122 (azorubine or carmoisine)
E124 (ponceau 4R)
E129 (allura red)
These colourings are used in many foods, including soft drinks, sweets, cakes and ice cream, so always read the labels – more to come on label reading in a future blog.
The easiest way to see how foods may be affecting your kids is to keep a food diary. Write down the food/s eaten, time of day and any behavioural changes noted after mins/hrs of time. A five-seven day diary will show you a pattern, and if things are showing up, discuss with your Paediatrician, GP or naturopath/nutritionist.
Neurodivergent children often eat a more restrictive diet with less fruits and vegetables and more fluffy carbs such as bread, pizza, cakes and biscuits. Good amounts of low GI carbohydrates (found in oats, lentils, rice, beans) and a balance of fruit and vegetables provide nutritious carbohydrates that are a steady source of energy – assisting with attention issues and brain fog.
Here are the key nutrients to focus on to best support the neurological function of your little one:
Magnesium - Great for a healthy stress response which in our neurodiverse little ones happens more often than in the average Joe. Children with ADHD or ASD also often have lower levels of magnesium.
Sources:
Nuts: almonds, pecans, cashews
Pumpkin seeds
Peanut butter
Brown rice
White potato with skin on
Green leafy veggies
Essential fatty acids (EFAs) - DHA is the MOST important omega-3 fatty acid for brain development and function, nerve tissue membranes and neural function.
Sources:
Flaxseed
Chia seeds
Mackerel (and other oily fish)
Hemp seeds
Wheatgerm
Vitamins B6 and B12 - B vits are essential for the making of neurotransmitters – those chemical messengers in the body that help our central nervous system communicate.
Sources:
B6: salmon, tuna, avocado, beef, turkey, milk, cheese, most vegetables, citrus fruit
B12: poultry, eggs, dairy, nutritional yeast, beef, sardines, organ meats
Vitamin E - Helps with the health of nerve cells and brain tissues.
Sources:
Sunflower seeds
Almonds
Peanut butter
Pumpkin
Red capsicum
Green leafy vegetables
Zinc - Assists in the modulation of nerve synapse activity, neural plasticity and an overall healthy brain. It’s also needed for digestive function.
Sources:
Red meat
Poultry
Chickpeas and other legumes
Cashews
Oats
Oysters
References:
1. Shareghfarid E, et al. Clin Nutr ESPEN. 2020;36:28-35.
2. Hontelez S, et al. Sci Rep. 2021;11(1):22205.
3. Abbasi K, et al. Food Sci Nutr. 2022;9;10(12):4339-4344.
4. Miller MD, et al. Environ Health. 2022;21(1):45.
5. Food Standards Agency UK. Available at: www.food.gov.uk/safety-hygiene/food-additives. Accessed on: 1 March 2024.
Managing meltdowns
Managing meltdowns…it’s overwhelm not a tantrum.
It’s not a tantrum, it’s overwhelm. These meltdowns are a response to such intense sensory overload or other frustrations, our neurodivergent kids become overwhelmed, their emotional bucket overflows. Our children work so hard every day to maintain balance in their worlds, but sometimes, the sensory pressures become too much too quickly and it all spills over.
The phrase ‘they went from 0-100’ is often used to describe these reactions, with observers seeing a calm child suddenly ‘lose it’. However, they have been sitting at 80-90 for a while and then the tiniest thing ‘tips them over’. But it is so important to acknowledge, this is not bad behaviour or a tantrum, they are in sensory overload and frustration.
Practical prevention strategies
Our children are not going to just magically cope next time we go shopping, to the pool or playground. We need to take time to plan ahead and set things up so our kids have a better chance of experiencing the busy outside world in a calm way.
Consider potential stress areas
Make a plan – help your child understand what to anticipate before heading out
Neurodivergent children track so much better with predictability. So many of the environments e.g. supermarkets, are the exact opposite of this
Head to the same store, walk the same path, shop for familiar foods. Or go to the same playground, at the same time of day and day of the week
Routine provides a reassuring rhythm for our kids, take them somewhere familiar
Think creatively – is there a better time to go shopping - when the kids are less tired, when it’s less crowded? Can we order online? Can we go to the pool outside of busy times?
Make sure they are well fed ahead of any activity and take extra snacks
Take along their favourite toy or comfort item
Where possible, be a little flexible with day:day routines to incorporate your child’s unique triggers and moods.
Handling overwhelm
It’s going to happen, despite planning and doing the best we can. We often have to try three or four things before we find what works and even then, something that worked yesterday won’t work today. Acknowledge the steps forward – building social and emotional skills alongside self-confidence is a huge job. It’s going to take a lot of patience, love and time.
So, when things go a little sideways, here are some tips to handling the overwhelm.
Go out armed and ready: headphones, sunglasses, snacks, water and a hat. Noise cancelling headphones/earbuds with fun, familiar music can help drown out the background noise of supermarkets and sunglasses and a hat can help lower the intensity of fluoro lighting. Snacks are a great distraction and can help your child feel grounded
And when the overwhelm happens
Take your child away from the stimulus – back to car or another quiet space where they can get away from it all. You may even need to bail on the activity and come back later
Reassure your child that they are safe, they are loved and they are OK
Work with them on breathing deeply and slowly once they are receptive to focusing on something
If pressure or touch helps, make sure you hug them, hold a hand or have a blanket or other comfort item in the car so they can find their safe place
If you’re in a group setting, take them to one side as calmy as you can. It is hard to stay calm in these situation as they are very stressful, but neurodiverse kids pick up on energy and will absorb and reflect it back very quickly. So, the calmer you are, the calmer they will become.
Most importantly, trust your intuition…always. You know your child better than anyone else :-).